For millennia humans have leveraged the power of breathing to improve their bodies and minds. Cultures and societies in all corners of the world understood and appreciated to some extent the beneficial effects that breathing can have in regulating our emotional and physical well-being. Despite being separated by continents and oceans, the ancient Greeks, Chinese, Indians, and other important cultures of humanity revered breath as the ultimate manifestation of life and regarded it as the foundational mechanism for healing the mind and body.
Despite thousands of years of exploring the effects of breathing and using its powers to improve mental and physical health, the art of breathing was largely lost in modern times. This was a consequence of the general marginalization of nearly every natural healing process by western medicine’s obsession with pharmacological intervention.
However, the renewed interest in alternative medicine coupled with a re-orientation of the scientific community’s focus on breathing has increased our understanding around breath and allowed us to appreciate its pivotal role in regulating nearly every core aspect of human physiology. One of them is mental health and our emotional state. This article aims to explore the intricate relationship between breathing and mental health and dissect the biological mechanism through which our mind, nervous system, and lungs are connected.
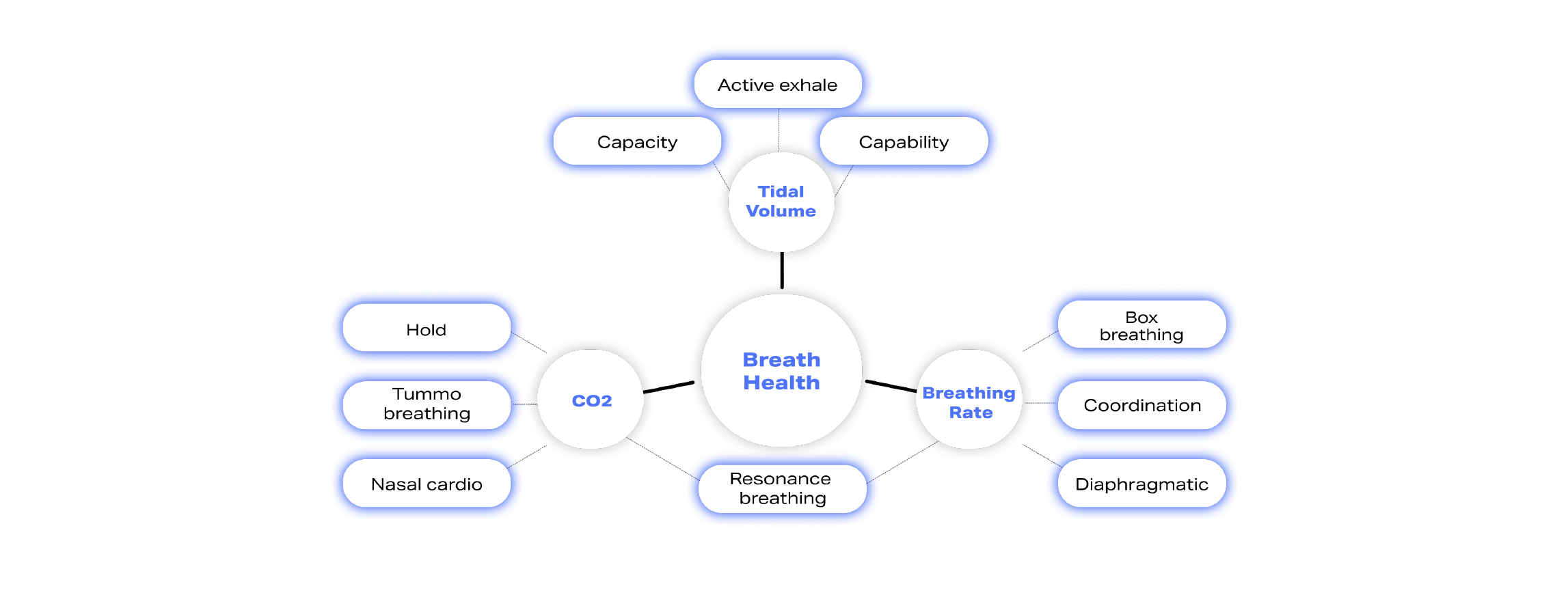
As a first step, let’s understand the fundamental biomarkers that characterize how healthy our breathing process is. These include
- End-tidal CO2: The amount of carbon dioxide we exhale,
- Tidal volume: The volume of air we exhale
- Breathing frequency: The number of breaths we take per minute.
These biomarkers reflect our breathing health because they constitute the basic mechanisms by which breathing affects nearly every process in our body, including our mental and emotional state. To understand this process, let’s examine, step by step, the sequence of events occurring when we experience stress.
How the Lung-Brain connection works
Step 1.
Stress is perceived through our brain after one or more of our sensory systems (e.g., our eyesight) is triggered.
Step 2.
The excitation of our brain engages our Autonomic Nervous System (ANS). ANS is divided into two parts, the Sympathetic Nervous System (SNS) and the Parasympathetic Nervous System (PNS). SNS causes us to go into “fight-or-flight” mode by engaging all the mechanisms required for movement, preservation, and fast reaction. PNS, on the other hand, causes feelings of relaxation and enables us to recover, digest, and heal. Experiencing psychological stress will almost immediately engage SNS and partially deactivate PNS.
Step 3.
Our brain is connected to our lungs and other critical organs through the vagus nerve, a principal conduit responsible for many of the psychosomatic processes in our body or the interaction between emotions and physical symptoms. The vagus nerve helps form the brain-lung axis. Specifically, SNS is connected to the upper part, whereas PNS is connected to the lower lungs. Due to the anatomy of the connection among lungs, SNS, and PNS, when psychological stress occurs, thus engaging SNS and partially deactivating PNS, we breath faster and shallower. On the contrary, when we deliberately breathe deeper and slower, we can activate PNS thanks to its connection to the lower part of our lungs and thus enable feelings of relaxation.
Step 4.
Due to the rise in breathing rate, the amount of air exhaled increases along with the amount of carbon dioxide (CO2) expelled through the body. As more CO2 leaves the body, CO2 circulating in the blood declines, causing a cascade of adverse effects as it is responsible for two critical biological functions. First, CO2 enables oxygen molecules to detach from hemoglobin (the substance in our blood responsible for transporting oxygen from our lungs across the body) and enter the cells that need them in order to produce energy. Second, CO2 regulates how narrow or wide our arteries are and the amount of blood delivered across the body. As a result, a reduction of CO2 levels in the blood will cause a tighter connection between oxygen molecules and hemoglobin, making it harder for oxygen to enter cells and narrowing the arteries, diminishing blood delivery to the brain and across the body.
Step 5.
Our brain understands the critical nature of CO2 for our physiology and will try to compensate for its changes. To achieve this, our brain is equipped with a sensory system that detects variations in CO2 concentrations and sends signals to our lungs to change the breathing rate accordingly.
Step 6.
When stress becomes constant, steps 1-5 become almost permanent, thus causing breathing to be faster and CO2 levels to be lower constantly. After years of exposure to this state, our brain’s CO2 sensory system becomes accustomed to lower blood CO2 levels and faster breathing, a condition also known as Chronic Hyperventilation Syndrome (CHS). As described above, lower blood CO2 levels reduce oxygen delivery to every cell and the brain. Insufficient brain oxygenation reduces cognitive capacity and mental clarity and increases the likelihood of mental disorders.
Step 7.
A constant state of rapid and shallow breathing (i.e., chest breathing) will engage SNS, the “fight-or-flight” part of our nervous system because SNS is connected to the upper part of our lungs.
The infographic below provides a visual representation of these steps. 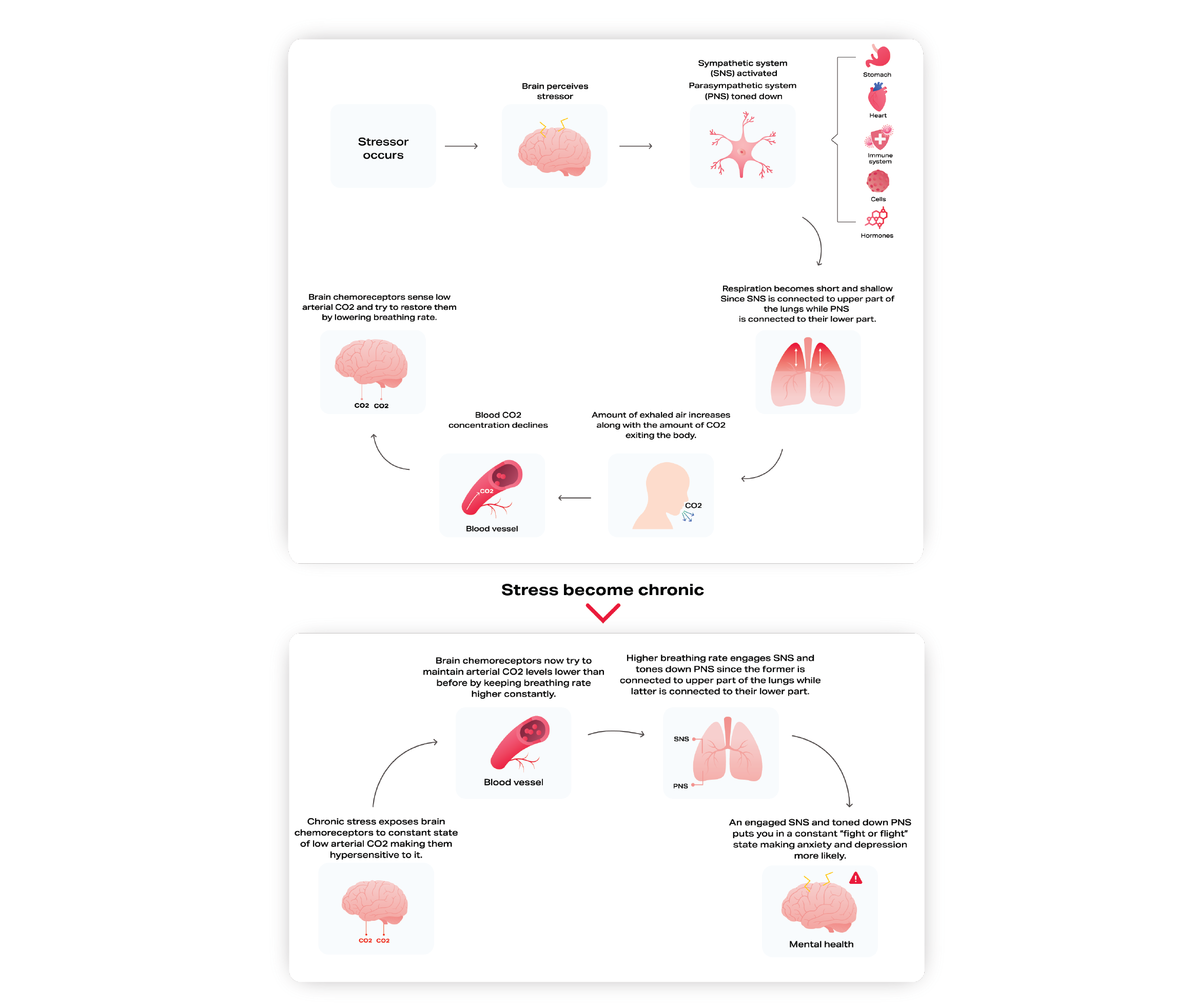
Breathwork: A way out of chronic stress
As described in steps 1-7, our stress response mechanism, nervous system, brain, and lungs are highly interconnected, and chronic stress can set them into a vicious self-fueling cycle. Simply put, stress causes our breathing to become unhealthy, whereas unhealthy breathing can cause or further promote psychological anxiety or mental disorder.
Based on steps 1-7, it becomes evident that breathing sits at the core of our brain and nervous system regulation. Luckily, breathing is the only core physiological function under our control. Thanks to the bilateral brain-lung connection, breathing changes can change how our brain and nervous system work. In other words, deliberate changes in our breathing patterns, a process also referred to by many as breathwork, can induce positive effects in our brain and nervous system and thus provide a viable solution to chronic stress.
Breathwork has many forms; each one targets a different part of our breathing apparatus. The graph below provides an overview of the most popular breathwork technics categorized based on the element of our breathing system they affect most.
Conclusion
Our brain, nervous system, and lungs are connected in an intricate relationship that can bring about a virtuous or vicious cycle for our mental health. In other words, breath can be the obstacle or the enabler of mental health. Understanding whether your breathing is positively or negatively affecting your stress levels and psychosomatic state is the first step toward leveraging the power of breathing to achieve a better quality of life. No matter the quality of your breathing, breathwork and the deliberate manipulation of your breathing can be a source of improvement of your mental state and habit that can improve your life.
Mental Health
