Menstruation is the cyclical sloughing of the uterine lining caused by changes in the balance of hormones secreted through a complex biological system that involves the female brain and ovaries (i.e., the hypothalamus, pituitary, and ovaries). The menstrual cycle is divided into two phases: The follicular or proliferative phase and the Luteal or secretory phase. The two phases of the menstrual cycle are dominated by the interaction of two fundamental hormones: Estrogen and Progesterone. Based on the different levels of estrogen and progesterone during the luteal and follicular phase, the menstrual cycle can be further divided into the following phases:
Early follicular
Late follicular
Ovulation
Early luteal
Mid luteal
Late luteal
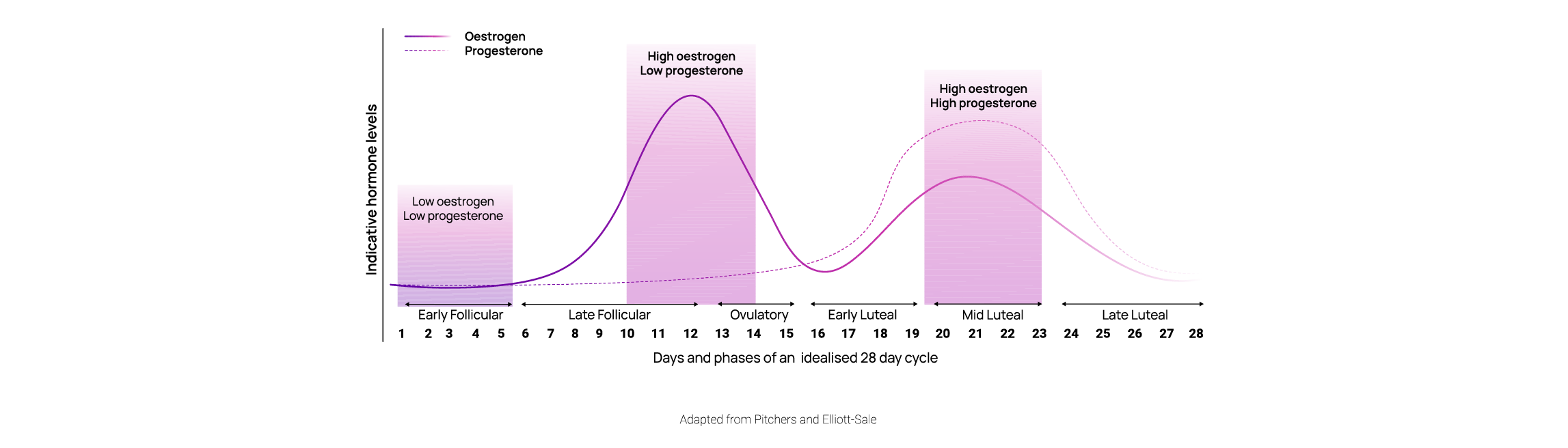
The shifting hormone levels bring about a cascade of changes that affect female respiration, metabolism, and by implication, several other critical systems, such as the brain. Many of these vital changes are reflected in the female breath and can be tracked using metabolic analysis. In the blog, we summarize the principal respiratory and metabolic changes that explain several of the most life-influencing phenomena of the menstrual cycle and determine the optimal nutrition and exercise for each phase. These changes can be categorized into the following groups:
- Respiratory changes
- Substrate utilization changes
Respiratory Changes
Respiratory changes refer to alterations in the mechanical movement of the lungs and affect the balance between oxygen and carbon dioxide in the blood. These changes in the lungs’ mechanical movement manifest through the elevation of breathing rate and reduction in tidal volume. In contrast, perturbation in the oxygen and carbon dioxide transfer is reflected in the reduction in end-tidal CO2.
- Breathing frequency: The number of breaths we take per minute
- Tidal volume: The volume of air we exhale
- End-tidal CO2: The amount of carbon dioxide we exhale
Overall, these three biomarkers reflect breathing health because they constitute the basic mechanisms by which breathing affects nearly every process in our body and reflects our psychosomatic state. A core biological processes bonded to breathing through a bilateral connection is the hormonal fluctuation during the menstrual cycle that gives rise to premenstrual syndrome, a well-known condition affecting women during the luteal phase and is responsible for several psychological and physiological discomforts. Approximately 50–80% of women report increased psychological symptoms such as anxiety, sadness and/or physical symptoms such as muscle aches and headaches during these phase. A growing number of studies now show that the biological mechanism triggering these psychological and physical symptoms share similar features with depression and anxiety disorders. As a result, they are reflected through similar changes in breathing mechanics. To understand this bilateral relationship, let’s examine, step by step, the sequence of events that allow the fluctuation of hormones during menstruation to influence the brain-lung axis.
Step 1.
A rise in progesterone levels during the luteal phase increases breathing rate, reduces tidal volume, and causes one to take shorter, faster, and shallower breaths.
Step 2.
Our brain is connected to our lungs and other critical organs through the vagus nerve, a principal conduit responsible for many of the psychosomatic processes in our body or the interaction between emotions and physical symptoms. The vagus nerve helps form the brain-lung axis and contains the main part of our Autonomic Nervous System (ANS). ANS is divided into the Sympathetic Nervous System (SNS) and the Parasympathetic Nervous System (PNS). SNS causes us to go into “fight-or-flight” mode by engaging all the mechanisms required for movement, preservation, and fast reaction. PNS, on the other hand, causes feelings of relaxation and enables us to recover, digest, and heal. SNS is connected to the upper part, whereas PNS is connected to the lower lungs. Due to the anatomy of the connection among lungs, SNS, and PNS, we breath faster and shallower when psychological stress occurs, thus engaging SNS and partially deactivating PNS. Conversely, when we breathe shallower and shorter, we activate the PNS and de-activate PNS despite the absence of an external stressor, a state during which breathing changes ignite sensations of stress.
Step 3.
Due to the rise in breathing rate, the amount of air exhaled increases along with the amount of carbon dioxide (CO2) expelled through the body. As more CO2 leaves the body, CO2 circulating in the blood declines, causing a cascade of adverse effects as it is responsible for two critical biological functions. First, CO2 enables oxygen molecules to detach from hemoglobin (the substance in our blood responsible for transporting oxygen from our lungs across the body) and enter the cells that need them to produce energy. Second, CO2 regulates how narrow or wide our arteries are and the amount of blood delivered across the body. As a result, reducing CO2 levels in the blood will cause a tighter connection between oxygen molecules and hemoglobin, making it harder for oxygen to enter cells and narrowing the arteries, diminishing blood delivery to the brain and across the body.
Step 4.
Our brain understands the critical nature of CO2 for our physiology and will set off a series of alarm mechanisms and compensatory processes to counteract the reduction in CO2 levels. To achieve this, our brain is equipped with a sensory system that detects variations in CO2 concentrations and sends signals to our lungs to change the breathing rate accordingly.
The above process summarizes how progesterone can inflict changes in our psychosomatic state by altering how our breathing apparatus functions. Studies have now shown that the perturbation of cardio-metabolic variables such as breathing rate and end-tidal CO2 positively correlate with the severity of psychosomatic PMS. This relationship underscores two elements:
- The critical role that breath plays in reflecting the pathophysiological state of the female body during menstruation
- The curative effects it can have on mitigating PMS symptoms thanks to the bilateral relationship that exists between respiratory variables and the brain-adrenal system.
These realities prove that breathing is the most influential (i.e., can induce psychosomatic changes) and insightful (i.e., can reveal information about our biological status) biological function in our control.
Substrate utilization changes
In addition to causing changes in the mechanical function of the female lungs and blood chemistry (i.e., perturbation of the CO2 levels), menstruation also changes the balance between fats and carbohydrates in female metabolism as well as the level of calorie expenditure. Several studies have indicated that the female body burns significantly more calories during the luteal than the follicular phase. The excitation of the autonomic nervous system and breathing rate during this phase is a common concomitant of elevated resting metabolic rate. It thus lends further support to the aforementioned breathing alterations occurring during the luteal phase. Moreover, the engagement of the sympathetic nervous system, in other words, the “fight-or-flight” mechanism, irrespective of the underlying trigger, is also almost always accompanied by a reduction in fat utilization and an increase in carbohydrate metabolism. This shift prepares the body for reacting effectively to threats as carbohydrates provide rapid energy availability as opposed to fat, which constitutes a slow-burning fuel source. The attenuation of fat oxidation and engagement of carbohydrate fuel sources among the different phases of the menstrual cycle can also be attributed to the lipolytic effects of estrogen. Spefically, estrogens are known to cause:
- Elevated lipoprotein lipase and hormone-sensitive lipase activity
- Elevated catecholamine-induced lipolysis (i.e., the process of dissolving fat molecules)
- Attenuation of lipogenic-related genes (i.e., the process of developing new fat molecules)
- Enablement of other hormones which promote fat oxidation glycogenesis at rest (i.e., storing of carbohydrates vs. burning them) and mitigate glycogenolysis during exercise (i.e., carbohydrate burn).
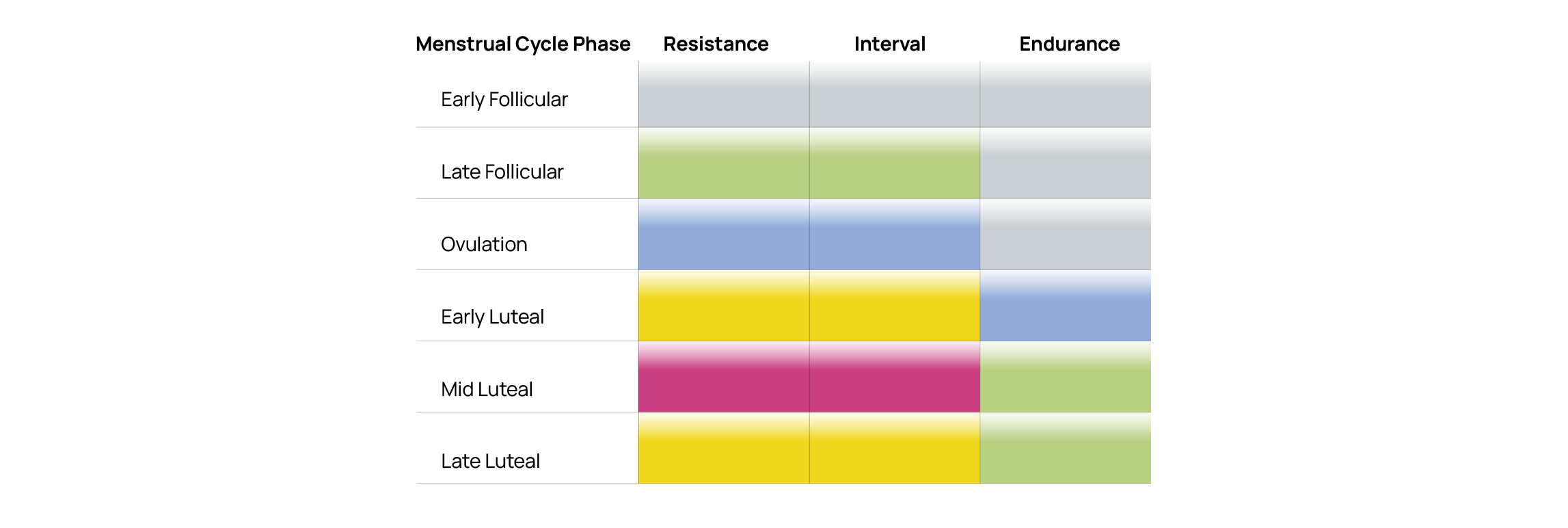
Overall, the interplay between estrogen and progesterone significantly affects energy consumption and fuel utilization during the menstrual cycle’s different phases, thus dictating optimal exercise and nutrition practices. The following table provides an overview of the recommended intensity spectrum during each menstrual cycle phase.

The following table provides a qualitative perspective of how appropriate each type of training is based on the phase of the menstrual cycle.
Conclusion
The menstrual cycle is a core biological clock that profoundly impacts breathing and metabolism. Understanding its mechanics can pave the way for better health, greater comfort throughout life, and higher ability to achieve fitness goals.
Longevity




